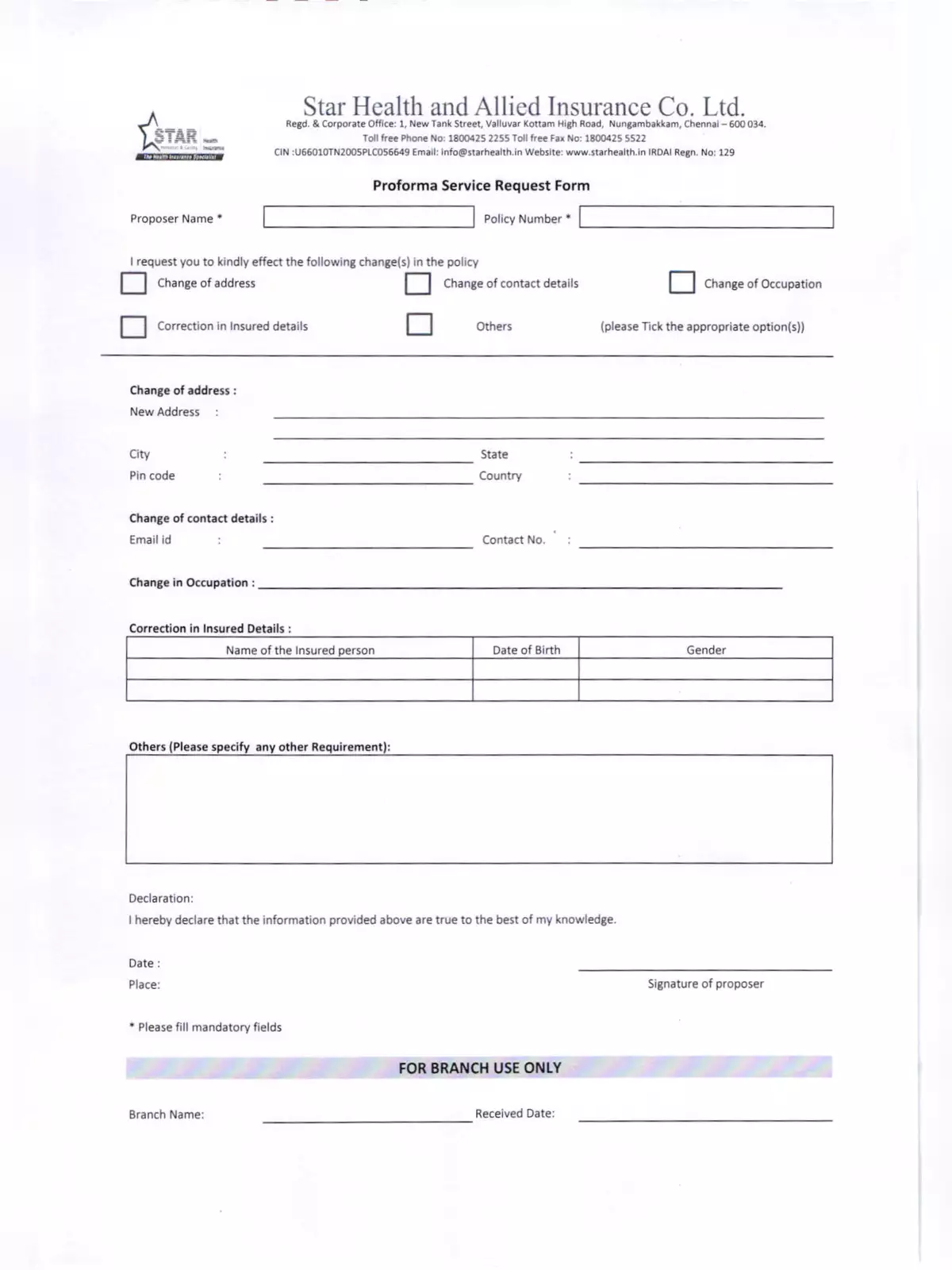
Star Health Proforma Service Request Form - Summary
With a vast network of over 5400 hospitals, Star Health & Allied Insurance ensures that claimants enjoy a seamless claims experience, minimizing any inconvenience related to medical expenses.
Documents Required for Claim Submission
- The original claim form, duly filled out and signed.
- A valid government-approved photo ID proof.
- A referral letter from a medical practitioner recommending hospitalization.
- A letter from your doctor detailing the tests, medications, and consultations, if necessary.
- Original invoices, receipts, and discharge cards from the hospital or medical practitioner.
- Original bills or receipts from the relevant pharmacies or druggists.
- Original copies of completed test reports and payment receipts.
- Case papers related to indoor treatment.
- The First Information Report and the Final Police Report, if applicable.
- If a post-mortem examination was conducted, keep the original report copy.
Cashless Treatment Option
In network hospitals, the Star Health Proforma Service Request Form allows for cashless treatment. This means that when you get treated at such hospitals, the bills are directly submitted to Star Health, and as a policyholder or claimant, you won’t need to pay anything upfront.
This makes healthcare more accessible and stress-free for everyone. For more details, you can download the **Star Health Proforma Service Request Form PDF** and enjoy a simple guide at your fingertips. Don’t miss the chance to enhance your healthcare experience—download the PDF today! 😊